The dynamics of the Pharmacy Benefit Manager (PBM) market are shaped by a complex interplay of various factors that influence how prescription drug benefits are managed. Understanding these dynamics is crucial for stakeholders, including insurers, pharmaceutical companies, healthcare providers, and patients, as they navigate the evolving landscape of healthcare.
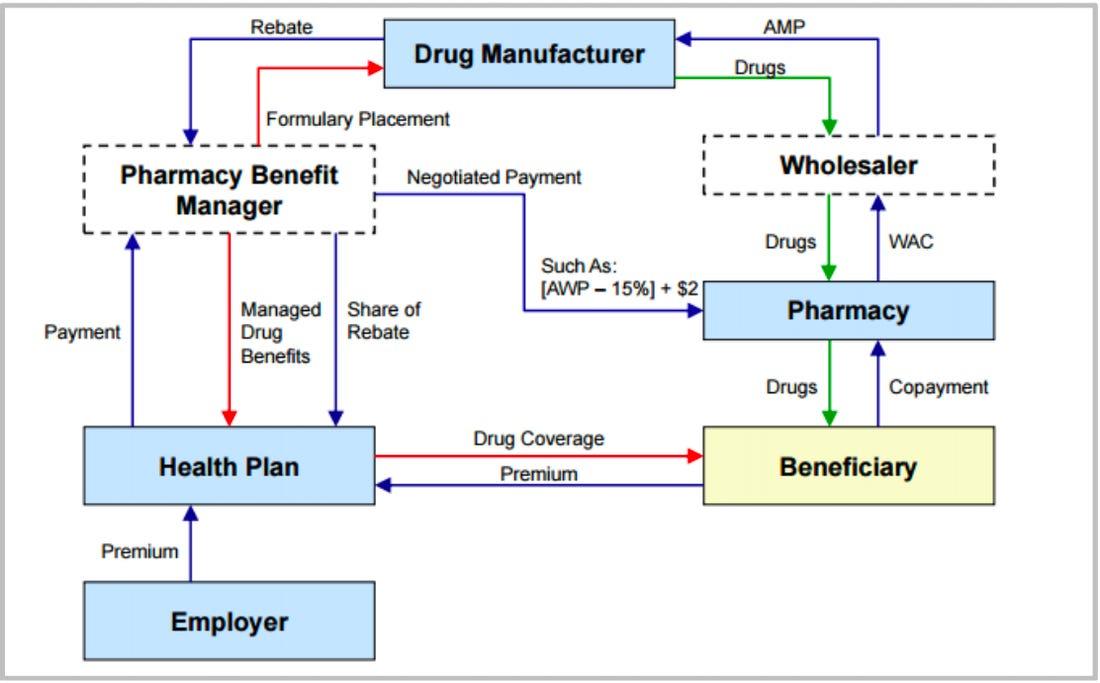
One of the most significant dynamics in the PBM market is the growing emphasis on cost management. As prescription drug prices continue to rise, both patients and payers are seeking effective strategies to mitigate these costs. PBMs serve as intermediaries that negotiate prices, secure rebates from manufacturers, and develop formularies that prioritize cost-effective medications. This role positions PBMs as essential partners in managing healthcare expenses, thus driving their influence in the market.
Another critical dynamic is the shift towards value-based care. The healthcare industry is increasingly focused on improving patient outcomes rather than merely increasing the volume of services provided. PBMs are adapting to this shift by implementing programs aimed at enhancing medication adherence and chronic disease management. By aligning their strategies with the principles of value-based care, PBMs can demonstrate their commitment to improving health outcomes, which strengthens their relationships with healthcare providers and payers.
Technological advancements also play a vital role in shaping the dynamics of the PBM market. The integration of data analytics, artificial intelligence, and telehealth solutions allows PBMs to streamline operations, improve decision-making, and offer personalized services. Through the use of real-time data, PBMs can better understand patient needs, optimize formularies, and create tailored programs that enhance patient care.
The regulatory pressures are further influencing PBM dynamics. Governments are implementing policies aimed at increasing transparency in drug pricing and ensuring equitable access to medications. PBMs that can navigate these regulatory changes while maintaining their core functions will likely thrive in this shifting landscape.
In brief, the dynamics of the Pharmacy Benefit Manager market are characterized by cost management, the transition to value-based care, technological innovations, and regulatory influences. By understanding and adapting to these dynamics, PBMs can enhance their effectiveness in managing prescription drug benefits and play a pivotal role in improving healthcare delivery.